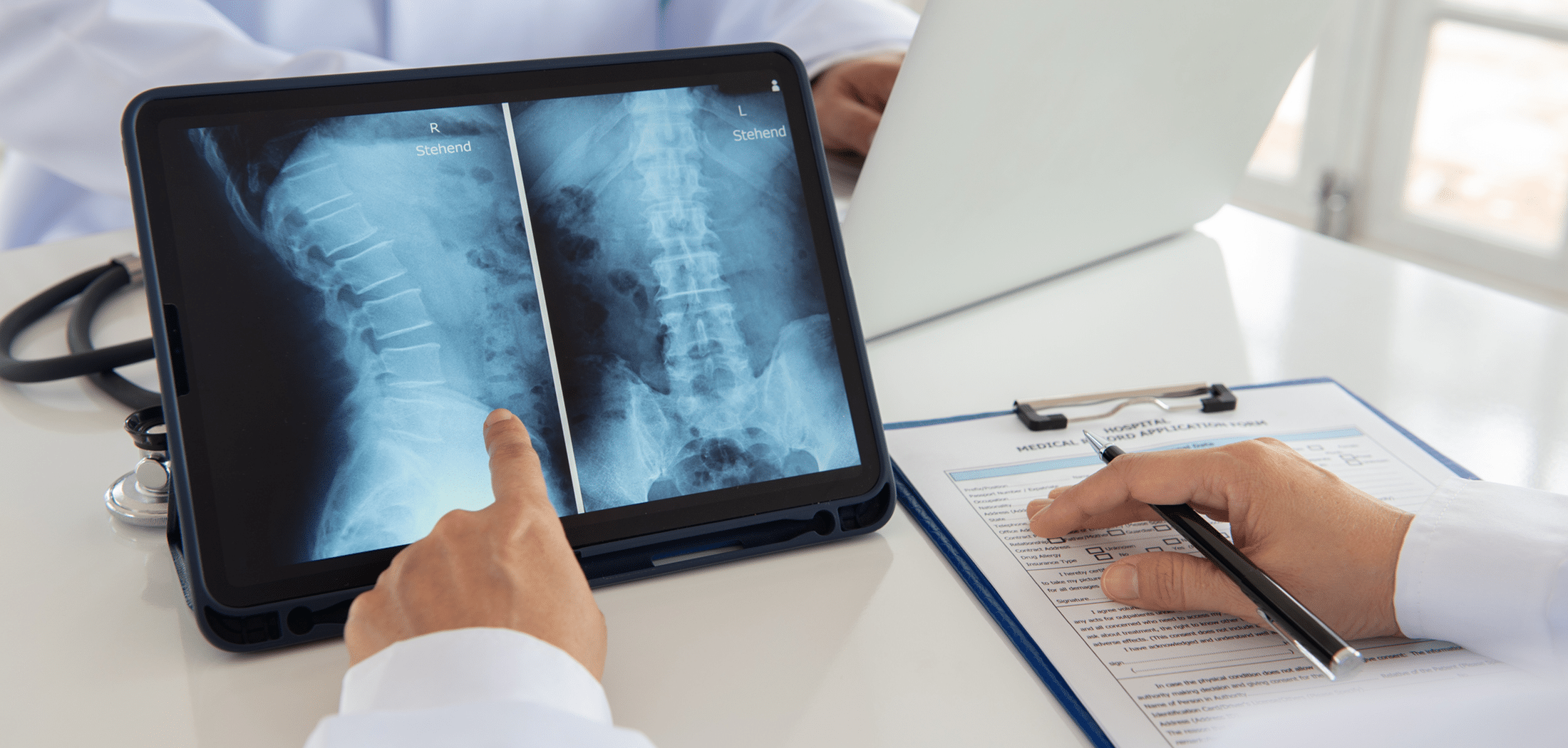
Advances in diagnostic imaging technology have greatly improved medical practitioners’ ability to see exactly what’s happening when an injury is not just skin deep.
In the first of a three-part blog series, I discuss some types of spinal cord injuries, explain what factors can lead to misdiagnosis, and outline what you should do if you suspect that you or a loved one has sustained a serious injury due to medical malpractice.
Types of Spinal Cord Injuries
Extending from the brainstem to the lower back, the spinal cord consists of a column of tightly bundled nerve cells, glia, nerve fibres, and blood vessels. It acts as a communication conduit that sends and receives information between the brain and body.
The spinal cord is surrounded by layers of tissue and cerebrospinal fluid in the spinal column to protect it from shock or injury. The spinal column contains 33 vertebrae (bone), discs (cartilage) and foramen (space for nerves, arteries, veins and lymphatic vessels).
Spinal cord injuries are often described as complete or incomplete.
If the spinal cord can still send some messages to or from the brain, a person will have an incomplete injury; this type of injury provides them with some level of sensation, function and/or muscle control below the site of the injury. A complete injury disrupts brain-body communication below the injury site causing full loss of sensation, function and muscle control.
Locating the site of the injury or damage to specific spinal nerves is often critical to understanding potential loss of function. In the neck, cervical spinal nerves (C1 to C7) control signals to the back of the head, neck, shoulders, arms, hands and the diaphragm. Thoracic spinal nerves (T1 to T12) in the upper to mid-back affect signals to the chest and back muscles and many organ systems.
Lumbar spinal nerves (L1 to L5) in the lower back are linked to signals for the lower abdomen and the back, the buttocks, some external genital organ parts, and some of the leg. Sacral spinal nerves (S1 to S5) in the lower back communicate signals to and from the thighs, lower legs, feet, most external genital organs, and the anal area.
The most common causes of spinal cord injuries are motor vehicle accidents and serious falls. Less common causes include traumatic injuries from violence, sports, industrial accidents or medical/surgical injury, disease, or other conditions.
Why might proper medical imaging be absent when diagnosing a potential spine injury?
First, the patient may not present in a way that leads a doctor to believe it is necessary. But while a patient actively undermining a doctor’s ability to accurately diagnose a condition is a failure that is not evidence of misdiagnosis as medical malpractice, if a doctor’s own bias plays a role in a misdiagnosis or delayed diagnosis, they could be liable for damages if serious harm results. For example, if a patient is intoxicated and mentioning or physically indicating they have neck or back pain, the medical practitioner may dismiss their complaints as being related to being inebriated or not investigate all possibilities fully.
Second, a community hospital may lack more advanced types of imaging equipment (such as MRIs) that could better indicate an injury or the extent of an injury. If the patient is not referred to a larger facility for this scan or not directed to take appropriate spinal precautions (particularly c-spine precautions), they may suffer harm.
Even if proper imaging is conducted, other system-related or cognitive errors may occur. Scanning the wrong segment of the spine could result in missed injuries. Less common, but possible, would be for a radiologist reading the scan to miss the injury due to negligence.
When is Misdiagnosis Medical Malpractice?
Misdiagnosis is not always evidence of negligence. Even highly trained medical practitioners are not held to a standard of perfection.
Medical practitioners with similar training and experience who are operating in similar conditions may honestly and reasonably reach a different diagnosis from one another. But if one of these practitioners reached this conclusion because they followed incorrect procedures or acted unreasonably while assessing, diagnosing, and treating the patient, it may be an indication that the standard of care owed to the patient has been breached due negligence.
Even if such a breach occurs, a medical malpractice action could only commence if the misdiagnosis or delayed diagnosis directly caused or contributed to the harm a patient suffered.
For instance, if this patient suffered a stable fracture (a break of the vertebrae that did not push or pull it out of alignment), they would not necessarily require surgical intervention, but would still require treatment. Without treatment, some stable fractures can become unstable (move out of alignment) and are much more likely to require surgery. Moreover, unstable fractures have an increased risk of complications that may affect the spinal cord.
If this misdiagnosis scenario resulted in unnecessary surgery or permanent loss of bodily function due to spinal cord damage, a case could be made that a breach of the standard of care due to negligence caused direct harm and loss to the patient.
What Can Be Done?
It is important for treating medical practitioners to understand the appropriate decision-making process for ordering imaging scans. For example, the Canadian C-spine rule was developed as a highly sensitive way to detect “acute C-spine injury among patients sustaining blunt trauma who are alert and stable but at risk for neck injury.”
Moreover, patients at risk for spinal cord injury should also be taught spinal fusion safety measures and techniques for spinal “pre-habilitation” as precautions if a diagnosis remains uncertain.
Unfortunately, even with defined processes and precautions, there may be times when a misdiagnosis or delayed diagnosis results in life-altering damage.
If you or a loved one has sustained a serious spinal cord injury and you believe medical malpractice may have played a role, it is in your best interest to speak to an experienced personal injury lawyer to discuss your legal rights.
When you contact the medical malpractice team at Howie, Sacks & Henry LLP for a no cost, no obligation initial consultation, we will listen to your story with great empathy, take time to answer your questions, and outline options available to you as you seek justice.
If we believe we can secure you a fair settlement or court award for damages, we will gladly offer to become your tireless advocate and trusted legal representative. By providing legal services on a contingency basis, we only receive compensation for our work if you receive compensation for your injuries.
A serious spinal injury can significantly change your life’s direction. At a moment when the future looks worryingly uncertain, let our team help you see that better days are ahead. Because at HSH LLP, Hope Starts Here. To learn more about how we can help you, contact me today.
Learn More
To learn more, please read Part 2 (Understanding Unstable Spinal Cord Fractures) and Part 3 (Spinal Cord Abscess: Identifying Symptoms and Risks of Delayed Diagnosis) of the series.